Summary: Researchers have identified functional connectivity problems in brain regions associated with visual processing and attention in Parkinson’s patients who experience visual hallucinations.
Source: RSNA.
Researchers have found that disconnections of brain areas involved in attention and visual processing may contribute to visual hallucinations in individuals with Parkinson’s disease, according to a new study published online in the journal Radiology. The disconnected brain areas seen on functional MRI (fMRI) may be valuable in predicting the development of visual hallucinations in patients with Parkinson’s disease.
Hallucinations are sensations that seem real but are created in a person’s mind. A person having a hallucination may see, hear or feel something that is not actually there. According to the National Parkinson Foundation, visual hallucinations can be a complication of Parkinson’s disease.
“Visual hallucinations in Parkinson’s disease are frequent and debilitating,” said study author Dagmar H. Hepp, M.D., from the Department of Neurology and the Department of Anatomy and Neurosciences at VU University Medical Center (VUMC) in Amsterdam, the Netherlands. “Our aim was to study the mechanism underlying visual hallucinations in Parkinson’s disease, as these symptoms are currently poorly understood.”
Studies using fMRI to investigate visual hallucinations in patients with Parkinson’s disease are rare and have been mainly limited to task-based methods using activities that involve visual stimulation or cognitive tasks. However, the authors note that the presence of visual hallucinations is strongly linked to the development of cognitive decline in patients with Parkinson’s disease. Cognitive deficits may influence a patient’s ability to perform specific tasks during an fMRI exam.
For this study, researchers used resting-state fMRI to examine the connectivity, or communication, between brain areas. Resting-state fMRI is a method of brain imaging that can be used to evaluate patients not performing an explicit task. The connectivity was measured in 15 patients with visual hallucinations, 40 patients without visual hallucinations, and 15 healthy controls by calculating the level of synchronization between activation patterns of different brain areas.
The results showed that in all the patients with Parkinson’s disease, multiple brain areas communicated less with the rest of the brain as compared to the control group. However, in patients suffering from visual hallucinations, several additional brain areas showed this decreased connectivity with the rest of the brain, especially those important in maintaining attention and processing of visual information.
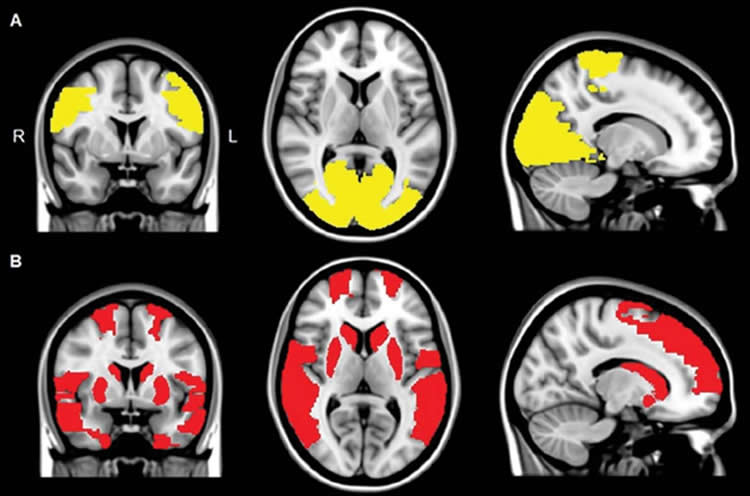
“We found that the areas in the brain involved in attention and visual processing were less connected to the rest of the brain,” said study author Menno M. Schoonheim, Ph.D., from the Department of Anatomy and Neurosciences at VUMC. “This suggests that disconnection of these brain areas may contribute to the generation of visual hallucinations in patients with Parkinson’s disease.”
While there are no direct therapeutic implications for patient care based on the research, the authors note that future studies could indicate whether techniques that could stimulate the areas with decreased connectivity could be helpful to treat visual hallucinations in people with Parkinson’s disease.
Funding: Funding provided by Stichting Parkinson Fonds, DutchParkinson Foundation, Graduate School Neurosciences Amsterdam Rotterdam, Netherlands.
Source: Linda Brooks – RSNA
Image Source: NeuroscienceNews.com image is adapted from the RSNA news release.
Original Research: Abstract for “Loss of Functional Connectivity in Patients with Parkinson Disease and Visual Hallucinations” by Dagmar H. Hepp, Elisabeth M. J. Foncke, Kim T. E. Olde Dubbelink, Wilma D. J. van de Berg, Henk W. Berendse, and Menno M. Schoonheim in Radiology. Published online September 27 2017 doi:10.1148/radiol.2017170438
[cbtabs][cbtab title=”MLA”]RSNA “Brain Disconnections May Contribute to Parkinson’s Hallucinations.” NeuroscienceNews. NeuroscienceNews, 27 September 2017.
<https://neurosciencenews.com/parkinsons-hallucinations-brain-disconnection-7593/>.[/cbtab][cbtab title=”APA”]RSNA (2017, September 27). Brain Disconnections May Contribute to Parkinson’s Hallucinations. NeuroscienceNews. Retrieved September 27, 2017 from https://neurosciencenews.com/parkinsons-hallucinations-brain-disconnection-7593/[/cbtab][cbtab title=”Chicago”]RSNA “Brain Disconnections May Contribute to Parkinson’s Hallucinations.” https://neurosciencenews.com/parkinsons-hallucinations-brain-disconnection-7593/ (accessed September 27, 2017).[/cbtab][/cbtabs]
Abstract
Loss of Functional Connectivity in Patients with Parkinson Disease and Visual Hallucinations
Purpose
To gain more insight into the pathophysiological mechanisms of visual hallucinations (VHs) in patients with Parkinson disease (PD) by analyzing whole-brain resting-state functional connectivity in PD patients with VH (hereafter, referred to as PD + VH patients) and without VH (hereafter, referred to as PD − VH patients) and control participants.
Materials and Methods
For this retrospective study, 15 PD + VH patients, 40 PD − VH patients, and 15 control participants from a prospective cohort study were included, which was approved by the local ethics board and written informed consent was obtained from all participants. Functional connectivity was calculated between 47 regions of interests, of which whole-brain and region-specific means were compared by using a general linear model with false discovery rate control for multiple comparisons.
Results
Whole-brain mean functional connectivity was significantly lower in PD patients compared with control participants, with regional decreases involving paracentral and occipital regions in both PD + VH and PD − VH patients (mean whole-brain functional connectivity in PD + VH vs PD − VH, 0.12 ± 0.01 [standard deviation] vs 0.14 ± 0.03, respectively; control participants, 0.15 ± 0.04; P < .05, corrected). In PD + VH patients, nine additional frontal, temporal, occipital, and striatal regions showed decreased functional connectivity compared with control participants (mean of these nine regions in PD + VH, PD − VH, and control participants: 0.12 ± 0.02, 0.14 ± 0.03, and 0.16 ± 0.04, respectively; P < .05, corrected). Resting-state functional connectivity was unrelated to motor performance (r = 0.182; P = .184) and related to cognitive deficits such as attention and perception (ρ, −0.555 and −0.558, respectively; P < .05).
Conclusion
The findings show a PD-related effect on resting-state functional connectivity of posterior and paracentral brain regions, whereas the presence of VH is associated with a more global loss of connectivity, related to attention and perception. These findings suggest that the pathophysiological mechanisms of VH in PD may include a global loss of network efficiency, which could drive disturbed attentional and visual processing.
“Loss of Functional Connectivity in Patients with Parkinson Disease and Visual Hallucinations” by Dagmar H. Hepp, Elisabeth M. J. Foncke, Kim T. E. Olde Dubbelink, Wilma D. J. van de Berg, Henk W. Berendse, and Menno M. Schoonheim in Radiology. Published online September 27 2017 doi:10.1148/radiol.2017170438






