Summary: Researchers have identified a new autoimmune disease that causes muscle pain and weakness. Large-histiocyte-related immune myopathy (LHIM), generates similar results to the condition rhabdomyolysis in blood chemistry samples. LHIM can effectively be treated with anti-inflammatory drugs to help reduce symptoms.
Source: WUSTL
A previously unknown autoimmune muscle disease involving the sudden onset of debilitating muscle pain and weakness has been identified by researchers at Washington University School of Medicine in St. Louis. The syndrome easily could be mistaken for other muscle diseases that require different treatment, so the findings are expected to help physicians treat patients appropriately, the researchers said.
“We observed only four patients in more than 20 years, so it’s very rare,” said senior author Alan Pestronk, MD, a professor of neurology, and of pathology and immunology. “It has never been described before, and it seems to be treatable, so it will be helpful for physicians to be aware of it. People don’t need to be afraid this is going to happen to them, but in the extremely rare event that it does, physicians should now have the tools to respond.”
The findings are available in the April 6 issue of the journal Neurology.
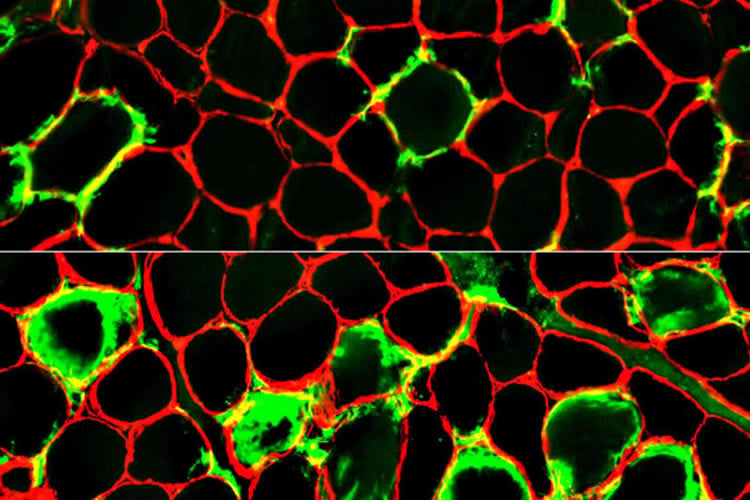
In 1996, Pestronk, who leads the university’s Neuromuscular Disease Clinic, was reviewing microscope slides of muscle from a patient with muscle pain and weakness when he saw something odd: Scavenger cells that normally feed on dead material were crowded around injured muscle fibers.
“This was an unusual enough situation that I kept it in my memory and stayed on the lookout for other cases like this,” Pestronk said.
Over the next 22 years, he encountered three more patients hospitalized for muscle pain and weakness whose biopsies showed muscle breakdown coupled with scavenger cells. By carefully analyzing the biopsies, Pestronk and colleagues discovered that the patients’ own muscles were under assault by immune scavenger cells known as histiocytes. They named the newfound syndrome large-histiocyte-related immune myopathy.
The disease also reflects a new way in which the immune system can damage muscle cells. Understanding how muscle fibers are damaged by immune cells could lead to ways to prevent damage.
“There are several immune muscle diseases where the primary damage you see under the microscope is muscle fiber breakdown. Each of these diseases has a different prognosis and requires a different treatment,” Pestronk said. “Physicians need to recognize the immune nature of this condition in order to treat it appropriately.”
Three of the patients improved when treated with immunomodulating therapy such as steroids and have not relapsed since. The fourth was undergoing cancer treatment when the muscle symptoms developed, and he died due to cancer shortly afterwards.
Further, while muscle pain and weakness brought the patients into the clinic, all four were also anemic and had other shared symptoms, so accurately diagnosing people with the syndrome would help doctors manage and treat their other symptoms as well, Pestronk said.
The condition also could be mistaken for rhabdomyolysis, a disease in which muscle fibers break down due to injury, overexercise or other reasons. This syndrome generates results similar to rhabdomyolysis on a blood chemistry workup. But people with rhabdomyolysis usually recover on their own, whereas the new syndrome can be effectively treated with anti-inflammatory drugs.
Funding: This study was supported by the Neuromuscular Research Fund.
Source:
WUSTL
Media Contacts:
Lucia Peixoto – WUSTL
Image Source:
The image is credited to ALAN PESTRONK.
Original Research: Closed access
“Immune myopathy with large-histiocyte-related myofiber necrosis”. Pestronk A, Sinha N, Alhumayyd Z, Ly C, Schmidt R, Bucelli R. Neurology. doi:10.1212/WNL.0000000000007260
Abstract
Immune myopathy with large-histiocyte-related myofiber necrosis
Abstract
Objective To describe the features of a new, pathologically distinctive, acquired myopathy with an unusual pattern of scattered necrotic muscle fibers that are neighbored, surrounded, or invaded, by large, often multinucleated, histiocytic cells.
Methods Retrospective review of records and muscle pathology of 4 patients.
Results Clinical features common to our patients included muscle pain and proximal, symmetric, moderate to severe, weakness in the arms and legs progressing over 1–4 weeks. Patients had other associated systemic disorders, including anemia in all, and hemophagocytic lymphohistiocytosis, hepatic disease, Raynaud phenomenon, metastatic cancer, and cardiomyopathy, in 1 patient each. Serum creatine kinase (CK) levels at presentation were very high, ranging from 10,000 to 102,000 U/L. Three patients improved within 3 months after treatment. Muscle pathology included scattered necrotic muscle fibers with cytoplasm that stained for C5b-9 complement, especially around fiber peripheries, pale on nicotinamide adenine dinucleotide and often dark on hematoxylin & eosin. Large, often multinucleated, cells with features of histiocytes, including anatomical features on electron microscopy and immunostaining for major histocompatibility complex Class I and histiocyte markers (HAM56, CD68, CD163, and S100), were usually closely apposed to the surface of, or invaded, necrotic myofibers.
Conclusions Patients with large-histiocyte-associated myopathy (LHIM) had a subacute onset of proximal predominant weakness, associated systemic disorders, very high serum CK, and a pathologically distinctive pattern of large histiocyte-associated muscle fiber necrosis. LHIM may be caused by an autoimmune, histiocyte-mediated attack directed against muscle fibers.






