Finding could have implications for other autoimmune disorders, such as type I diabetes.
Scientists from the Gladstone Institutes have discovered a way to prevent the development of multiple sclerosis (MS) in mice. Using a drug that blocks the production of a certain type of immune cell linked to inflammation and autoimmunity, the researchers successfully protected against the onset of MS in an animal model of the disease. The scientists say the next step is to test this strategy using other autoimmune disorders.
“We are very excited about these findings,” says Eric Verdin, MD, a senior investigator at Gladstone and co-senior author on the study. “In light of the significant effect the treatment had on inflammation, the implications of these results will likely extend beyond multiple sclerosis to other types of autoimmune disorders. We are particularly interested in testing this in type I diabetes given the similar pathways involved, and we are already seeing very promising results in preliminary experiments.”
In the immune system, two kinds of T cells strike a delicate balance—T helper cells (Th17) activate the immune system, protecting against infections and cancers, while regulatory T cells (Tregs) suppress the system, keeping it in check. A disparity between these cell types, when there are too many Th17 and not enough Tregs, can lead to a hyperactive immune system, resulting in inflammation, tissue damage, and autoimmune disease.
In the current study, published in the Journal of Experimental Medicine, the researchers discovered that an important regulatory protein, sirtuin 1 (SIRT1), is involved in the production of Th17 cells. By blocking this protein, the scientists can protect against the onset of autoimmunity. SIRT1 also has a negative impact on Treg maturation and maintenance, so inhibiting its expression simultaneously enhances the production of Tregs and suppresses the creation of Th17.
To test this effect on disease, the researchers used a mouse model of MS and treated the animals with a drug that inhibits SIRT1. Typically, MS-model mice experience severe motor problems, eventually leading to paralysis, but when they were given the drug the mice behaved perfectly normally. Moreover, the treated animals showed no signs of inflammation or cell damage in their spines, classic markers for MS.
In contrast with the current research, SIRT1 is typically thought of as having anti-inflammatory properties, and compounds that increase SIRT1—like resveratrol—have been proposed as a way to delay aging. However, first author Hyungwook Lim, PhD, a postdoctoral fellow at Gladstone, says the new research suggests that the protein’s effects are more complicated.
“The conventional theory has been that you should activate SIRT1 to improve health and longevity, but we show that this can have negative consequences,” says Dr. Lim. “Instead, we think the role of SIRT1 very much depends on the type of tissue being targeted. For instance, in immune cells, instead of being anti-inflammatory SIRT1 appears to have a pro-inflammatory role, which makes it a prime target to treat autoimmune disorders.”
Other Gladstone investigators on the study include Jae Kyu Ryu, Mingjian Fei, Intelly Lee, Kotaro Shirakawa, Herbert Kasler, Hye-Sook Kwon, Katerina Akassoglou, and Melanie Ott, who was a co-senior author on the paper. Scientists from the University of California San Francisco, Scripps Research Institute, Buck Institute for Research on Aging, National Institute of Infectious Diseases Japan, German Cancer Research Center, New York University School of Medicine, and Howard Hughes Medical Institute also took part in the research.
Funding: Funding was provided by the Kurtzig and Mulholland families, the National Center for Research Resources, and the National Center for Biotechnology Information.
Source: Dana Smith – Gladstone Institute
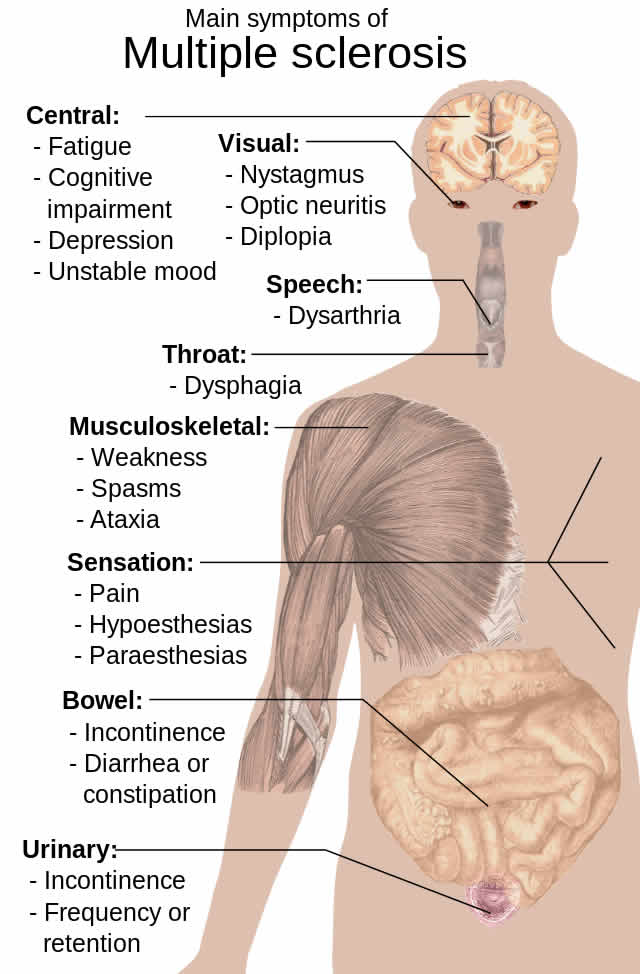
Image Source: Image credited to Mikael Häggström.
Original Research: Abstract for “SIRT1 deacetylates RORγt and enhances Th17 cell generation” by Hyung W. Lim, Seung Goo Kang, Jae Kyu Ryu, Birgit Schilling, Mingjian Fei, Intelly S. Lee, Amanuel Kehasse, Kotaro Shirakawa, Masaru Yokoyama, Martina Schnölzer, Herbert G. Kasler, Hye-Sook Kwon, Bradford W. Gibson, Hironori Sato, Katerina Akassoglou, Changchun Xiao, Dan R. Littman, Melanie Ott, and Eric Verdin in Journal of Experimental Medicine. Published online April 27 2015 doi:10.1084/jem.20132378
Abstract
SIRT1 deacetylates RORγt and enhances Th17 cell generation
The balance of effector and regulatory T cell function, dependent on multiple signals and epigenetic regulators, is critical to immune self-tolerance. Dysregulation of T helper 17 (Th17) effector cells is associated with multiple autoimmune diseases, including multiple sclerosis. Here, we report that Sirtuin 1 (SIRT1), a protein deacetylase previously reported to have an antiinflammatory function, in fact promotes autoimmunity by deacetylating RORγt, the signature transcription factor of Th17 cells. SIRT1 increases RORγt transcriptional activity, enhancing Th17 cell generation and function. Both T cell–specific Sirt1 deletion and treatment with pharmacologic SIRT1 inhibitors suppress Th17 differentiation and are protective in a mouse model of multiple sclerosis. Moreover, analysis of infiltrating cell populations during disease induction in mixed hematopoietic chimeras shows a marked bias against Sirt1-deficient Th17 cells. These findings reveal an unexpected proinflammatory role of SIRT1 and, importantly, support the possible therapeutic use of SIRT1 inhibitors against autoimmunity.
“SIRT1 deacetylates RORγt and enhances Th17 cell generation” by Hyung W. Lim, Seung Goo Kang, Jae Kyu Ryu, Birgit Schilling, Mingjian Fei, Intelly S. Lee, Amanuel Kehasse, Kotaro Shirakawa, Masaru Yokoyama, Martina Schnölzer, Herbert G. Kasler, Hye-Sook Kwon, Bradford W. Gibson, Hironori Sato, Katerina Akassoglou, Changchun Xiao, Dan R. Littman, Melanie Ott, and Eric Verdin in Journal of Experimental Medicine. Published online April 27 2015 doi:10.1084/jem.20132378






