Summary: A new study reports people can show early symptoms of multiple sclerosis up to five years before full onset of the disease.
Source: University of British Columbia.
People with multiple sclerosis can show signs of something wrong five years before the onset of disease, much earlier than previously thought, according to a new analysis of health records from people with the condition.
The new research, published today in Lancet Neurology, is a first step to identifying red flags to help doctors screen for the disease and start interventions earlier. This could point researchers in a new direction for finding the root cause of the disease.
“Proving that people with multiple sclerosis have already changed their behaviour in the five years before even the earliest medical recognition of the condition is very important because it means we have to look beyond those five years to understand how it is caused,” said Helen Tremlett, senior author of the study and a professor in the department of medicine at the Djavad Mowafaghian Centre for Brain Health.
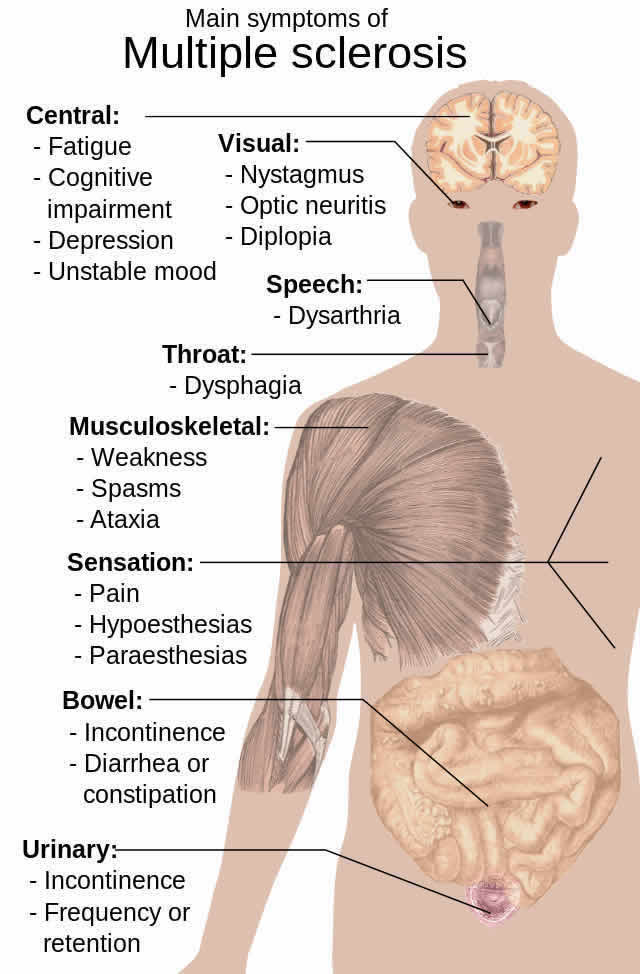
Multiple sclerosis is thought to be an autoimmune disease where the body attacks the protective coating, known as myelin, around brain cells. Once a person is diagnosed with multiple sclerosis, a physician will try to pinpoint the onset of the disease, sometimes known as the patient’s first demyelinating event, and can include problems with vision or motor control.
The researchers examined health records of 14,000 people with multiple sclerosis from B.C., Saskatchewan, Manitoba and Nova Scotia over a 20-year period and compared them to the health records of 72,000 people without the disease. They were looking for something called a prodrome, an early set of symptoms that can indicate the onset of a disease.
Prodromes have been identified for other neurological conditions like Alzheimer’s and Parkinson’s diseases. The recognition of these prodromes has provided clues about how the diseases might begin and has stimulated new research into causes or triggers.
This study of patients from across Canada revealed that there is a phase where people begin to show symptoms before multiple sclerosis is medically recognized. During this phase patients tend to visit their physicians, be admitted to a hospital and fill prescriptions more than the general population.
“There’s something going on here that makes this population of people unique,” said José Wijnands, first author of the manuscript, a postdoctoral fellow and a Michael Smith Foundation for Health Research trainee.
“When other degenerative brain diseases have a prodrome, it suggests that something may be happening,” said Tremlett. “We hope to uncover what this might be in multiple sclerosis.”
Going forward, the team of researchers will try to understand why these patients had been using the health-care system differently, and whether there are trends in illnesses reported and prescriptions filled that point to a specific set of symptoms that doctors could use to help identify multiple sclerosis earlier.
Funding: This research was funded by the National Multiple Sclerosis Society, a U.S.-based charity, but the data comes from Canada where researchers can access data on health-care system use across the country.
Source: Heather Amos – University of British Columbia
Image Source: NeuroscienceNews.com image is in the public domain.
Original Research: Abstract for “Health-care use before a first demyelinating event suggestive of a multiple sclerosis prodrome: a matched cohort study” by José M A Wijnands, PhD, Elaine Kingwell, PhD, Feng Zhu, MSc, Yinshan Zhao, PhD, Tanja Högg, MSc, Karen Stadnyk, MSc, Okechukwu Ekuma, MSc, Xinya Lu, PhD, Charity Evans, PhD, John D Fisk, PhD, Prof Ruth Ann Marrie, MD, and Prof Helen Tremlett in Lancet Neurology. Published online April 20 2017 doi:10.1016/S1474-4422(17)30076-5
[cbtabs][cbtab title=”MLA”]University of British Columbia “Medical History Reveals Multiple Sclerosis Begins to Impact Patients Sooner.” NeuroscienceNews. NeuroscienceNews, 21 April 2017.
<https://neurosciencenews.com/multiple-sclerosis-impact-time-6468/>.[/cbtab][cbtab title=”APA”]University of British Columbia (2017, April 21). Medical History Reveals Multiple Sclerosis Begins to Impact Patients Soonere. NeuroscienceNew. Retrieved April 21, 2017 from https://neurosciencenews.com/multiple-sclerosis-impact-time-6468/[/cbtab][cbtab title=”Chicago”]University of British Columbia “Medical History Reveals Multiple Sclerosis Begins to Impact Patients Sooner.” https://neurosciencenews.com/multiple-sclerosis-impact-time-6468/ (accessed April 21, 2017).[/cbtab][/cbtabs]
Abstract
Health-care use before a first demyelinating event suggestive of a multiple sclerosis prodrome: a matched cohort study
Background
Degenerative processes in neurodegenerative diseases can start years before clinical manifestation. We aimed to establish whether a multiple sclerosis prodromal period exists by examining patterns of health-care use before a first demyelinating event.
Methods
In this matched cohort study, we used data from linked health administrative and clinical databases from four Canadian provinces (British Columbia, Saskatchewan, Manitoba, and Nova Scotia) to compare hospital, physician, and prescription use data from people with multiple sclerosis and matched general population controls in the 5 years before the first demyelinating disease claim (health administrative index date) or clinically reported symptom onset (clinical index date). Rate ratios (RRs) were estimated using negative binomial regression and combined across provinces using random effect models. The primary outcome was all-cause use of health care during each of the 5 years before the health administrative or clinical index date.
Findings
The health administrative cohort included 14 428 multiple sclerosis cases and 72 059 matched controls for whom data were available between April, 1984, and April, 2014. Annual health-care use increased steadily between 5 years and 1 year before the first demyelinating disease claim in people with multiple sclerosis compared with controls (from RR 1·26 [95% CI 1·16–1·36] to 1·78 [1·50–2·10] for hospital admissions; from 1·24 [1·16–1·32] to 1·88 [1·72–2·07] for physician claims; and from 1·23 [1·06–1·41] to 1·49 [1·41–1·59] for prescriptions, assessed as drug classes). Similar patterns for physician claims and prescriptions were observed in the cohort with available clinical symptom onset (3202 individuals with multiple sclerosis and 16 006 controls), although the differences in use in each of the 5 years mostly did not reach statistical significance.
Interpretation
More frequent use of health care in patients with multiple sclerosis than in controls in the 5 years before a first demyelinating event, according to health administrative data, suggests the existence of a measurable multiple sclerosis prodrome. These findings have clinical and research implications, including the establishment of an earlier window of opportunity to identify and potentially treat multiple sclerosis.
Funding
National Multiple Sclerosis Society.
“Health-care use before a first demyelinating event suggestive of a multiple sclerosis prodrome: a matched cohort study” by José M A Wijnands, PhD, Elaine Kingwell, PhD, Feng Zhu, MSc, Yinshan Zhao, PhD, Tanja Högg, MSc, Karen Stadnyk, MSc, Okechukwu Ekuma, MSc, Xinya Lu, PhD, Charity Evans, PhD, John D Fisk, PhD, Prof Ruth Ann Marrie, MD, and Prof Helen Tremlett in Lancet Neurology. Published online April 20 2017 doi:10.1016/S1474-4422(17)30076-5






