Medulloblastoma subgroups can be identified using imaging techniques, allowing early intervention.
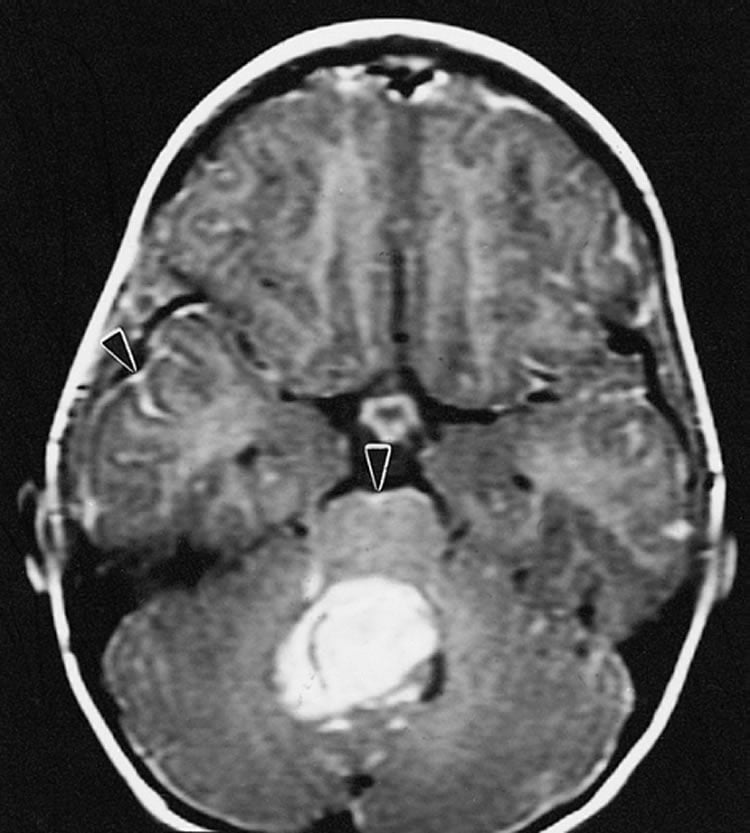
Medulloblastoma, the most commonly occurring malignant brain tumor in children, can be classified into four subgroups–each with a different risk profile requiring subgroup-specific therapy. Currently, subgroup determination is done after surgical removal of the tumor. Investigators at Children’s Hospital Los Angeles have now discovered that these subgroups can be determined non-invasively, using magnetic resonance spectroscopy (MRS). The paper will be published online by the journal Neuro-Oncology on August 7.
“By identification of the tumor subgroup at the time of diagnosis, we will be able to begin specific therapy earlier,” said Shahab Asgharzadeh, MD, of The Saban Research Institute of Children’s Hospital Los Angeles, principal investigator on the study. Asgharzadeh is also an associate professor of Pediatrics and Pathology at the Keck School of Medicine of the University of Southern California (USC).
Treatment for medulloblastoma includes surgery, chemotherapy and radiation, with 5-year survival rates ranging from 30 to 90 percent depending upon risk profile. A recent discovery identified four subtypes of medulloblastoma (SHH, WNT, Group 3 and Group 4) with level of risk and clinical outcomes for each subtype varying significantly. Currently, classification requires surgical removal of the tumor followed by laboratory analysis of the tumor tissue. Given the clinical importance of subgroup determinations, a fast, reliable and easily accessible method could have a significant effect on the outcomes of children with this disease.
“MR spectroscopy is widely available, noninvasive and provides information on cellular metabolism, which is different in healthy and diseased tissue,” said Stefan Bluml, PhD, investigator at The Saban Research Institute of CHLA and first author of the study. Bluml is also an associate professor of Research, Radiology and Biomedical Engineering at the Viterbi School of Engineering at USC.
Using frozen tumor tissue from 30 patients diagnosed with medulloblastoma, investigators performed subgroup analysis using standard techniques. These patients also had MRS performed at the time of diagnosis. With a screening panel composed of five metabolites, investigators found that the spectra for subgroups revealed distinct metabolic features, allowing them to differentiate subgroups SHH, WNT from Groups 3 and 4.
Clinical trials are being developed to incorporate molecular subgroups into risk and treatment stratifications. The ease of obtaining MRS at the time of diagnosis should allow its incorporation into future clinical trials aimed at validating this technique to improve diagnostic classification and, ultimately, improve outcomes in children with medulloblastoma.
Additional contributors include co-first author Ashley S. Margol, Richard Sposto, Rebekah J. Kennedy, Nathan J. Robison, Marzieh Vali, Long T. Hung, Sakunthala Muthugounder, Anat Erdreich-Epstain, Floyd H. Gilles, Alexander R. Judkins, Mark D. Krieger, Girish Dhall and Marvin D. Nelson, of Children’s Hospital Los Angeles and the Keck School of Medicine of USC; and Jonathan L. Finlay, Nationwide Children’s Hospital, Columbus, OH.
Funding: Funding was provided in part by the National Institutes of Health (grant CA009659-18), the American Cancer Society, Alex’s Lemonade Stand Foundation and the Rudi Schulte Research Institute.
Source: Ellin Kavanagh – Children’s Hospital of Los Angeles
Image Source: The image is in the public domain
Original Research: Abstract for “Molecular subgroups of medulloblastoma identification using noninvasive magnetic resonance spectroscopy” by Stefan Blüml, Ashley S. Margol, Richard Sposto, Rebekah J. Kennedy, Nathan J. Robison, Marzieh Vali, Long T. Hung, Sakunthala Muthugounder, Jonathan L. Finlay, Anat Erdreich-Epstein, Floyd H. Gilles, Alexander R. Judkins, Mark D. Krieger, Girish Dhall, Marvin D. Nelson, and Shahab Asgharzadeh in Neuro-Oncology. Published online August 8 2014 doi:10.1093/neuonc/nov097
Abstract
Molecular subgroups of medulloblastoma identification using noninvasive magnetic resonance spectroscopy
Background Medulloblastomas in children can be categorized into 4 molecular subgroups with differing clinical characteristics, such that subgroup determination aids in prognostication and risk-adaptive treatment strategies. Magnetic resonance spectroscopy (MRS) is a widely available, noninvasive tool that is used to determine the metabolic characteristics of tumors and provide diagnostic information without the need for tumor tissue. In this study, we investigated the hypothesis that metabolite concentrations measured by MRS would differ between molecular subgroups of medulloblastoma and allow accurate subgroup determination.
Methods MRS was used to measure metabolites in medulloblastomas across molecular subgroups (SHH = 12, Groups 3/4 = 17, WNT = 1). Levels of 14 metabolites were analyzed to determine those that were the most discriminant for medulloblastoma subgroups in order to construct a multivariable classifier for distinguishing between combined Group 3/4 and SHH tumors.
Results Medulloblastomas across molecular subgroups revealed distinct spectral features. Group 3 and Group 4 tumors demonstrated metabolic profiles with readily detectable taurine, lower levels of lipids, and high levels of creatine. SHH tumors showed prominent choline and lipid with low levels of creatine and little or no evidence of taurine. A 5-metabolite subgroup classifier inclusive of creatine, myo-inositol, taurine, aspartate, and lipid 13a was developed that could discriminate between Group 3/4 and SHH medulloblastomas with excellent accuracy (cross-validated area under the curve [AUC] = 0.88).
Conclusions The data show that medulloblastomas of Group 3/4 differ metabolically as measured using MRS when compared with SHH molecular subgroups. MRS is a useful and accurate tool to determine medulloblastoma molecular subgroups.
“Molecular subgroups of medulloblastoma identification using noninvasive magnetic resonance spectroscopy” by Stefan Blüml, Ashley S. Margol, Richard Sposto, Rebekah J. Kennedy, Nathan J. Robison, Marzieh Vali, Long T. Hung, Sakunthala Muthugounder, Jonathan L. Finlay, Anat Erdreich-Epstein, Floyd H. Gilles, Alexander R. Judkins, Mark D. Krieger, Girish Dhall, Marvin D. Nelson, and Shahab Asgharzadeh in Neuro-Oncology. Published online August 8 2014 doi:10.1093/neuonc/nov097






