Could hypnosis help to reduce the psychological trauma associated with “awake craniotomy” for brain cancers? A new “hypnosedation” technique offers a new alternative for patients undergoing awake surgery for gliomas, suggests a study in the January issue of Neurosurgery, official journal of the Congress of Neurological Surgeons.
Initial evaluation shows a high rate of successful hypnosis in patients undergoing “awake craniotomy” for brain cancer (glioma), report Dr. Ilyess Zemmoura of Centre Hospitalier Universitaire de Tours, France, and colleagues. They believe that hypnosedation might be especially valuable in patients with more advanced brain cancers.
Hypnosis Provides Sedation and Relaxation during ‘Awake’ Brain Surgery
Dr. Zemmoura and colleagues evaluated their hypnosis technique in 37 patients undergoing awake craniotomy, mainly for low-grade gliomas, between 2011 and 2015. In awake craniotomy, the patient is sedated but conscious so as to be able to communicate during the operation. This helps the surgeon navigate safely to the tumor without damaging the “eloquent cortex”–critical areas of the brain involved in language or movement.
Preparation for hypnosis began a few weeks before surgery. The anesthesiologist/hypnotist met with the patient to carry out a short hypnosis session and teach the patient how to create a “safe place”–an imaginary place where they can feel safe and effective.
In the operating room, patients were placed in a hypnotic trance; for example, they were instructed to “let go” and to “separate the mind and body.” The hypnotic experience was progressively enhanced during the first steps of surgery, including specific instructions and imagery for each potentially unpleasant or painful step of the surgery.
The 37 patients underwent a total of 43 surgeries with hypnosedation (including repeat surgeries in patients with recurrent gliomas). Hypnosis failed in six patients, who underwent standard “asleep-awake-asleep” anesthesia. Another two patients decided not to undergo hypnosis.
When successful, hypnosis was a reliable and reproducible method for awake surgery, with questionnaire assessments showing little or no negative psychological impact. Rather than any measure of individual “hypnotizability,” the success of hypnosis seemed to be most strongly related to the patients’ motivation and determination.
Hypnosedation seemed to reduce the impact of unpleasant events during surgery. Some patients reported high stress levels, but this did not appear to affect their subjective experience of hypnosis. The one patient who showed signs of posttraumatic stress disorder after surgery had a particularly good experience with hypnosis.
For patients, the most unpleasant parts of surgery were steps involving noise and vibration. Pain seemed to decrease as the level of hypnosis deepened. Only two patients said they would not choose to undergo hypnosedation if they had to undergo a second awake craniotomy.
An important advantage of hypnosedation is that it allows the patient to remain awake throughout surgery. This avoids the need to awaken the patient in the middle of standard “asleep-awake-asleep” anesthesia–which can be especially challenging in patients with high-grade gliomas. The authors note that their experience included successful hypnosedation in two patients with high-grade gliomas.
While the initial evaluation is encouraging, Dr. Zemmoura and colleagues note that it provides no evidence that hypnosedation is superior to standard anesthesia. They also emphasize the considerable investment of time and commitment needed to prepare for and carry out their hypnosis technique: “It requires intense involvement and long training of the whole team, including the patient.”
Source: Connie Hughes – WK Health
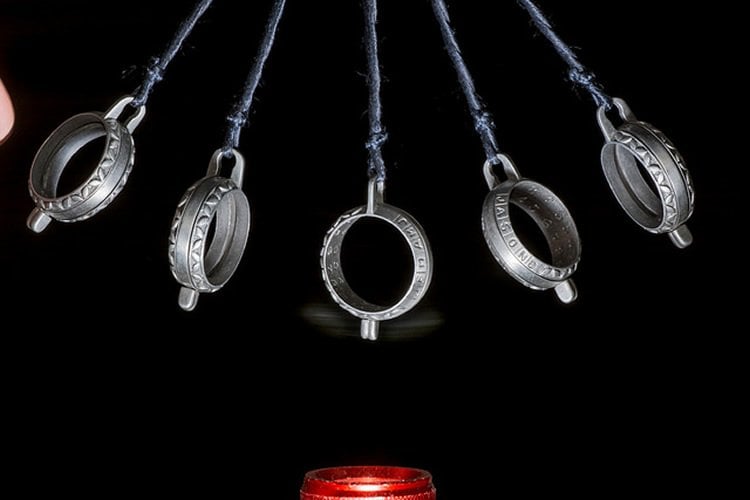
Image Source: The image is credited to Ray Scrimgeour and is licensed CC BY 2.0
Original Research: Full open access research for “Hypnosis for Awake Surgery of Low-grade Gliomas: Description of the Method and Psychological Assessment” by Zemmoura, Ilyess MD, PhD; Fournier, Eric MD; El-Hage, Wissam MD, PhD; Jolly, Virginie ST; Destrieux, Christophe MD, PhD; and Velut, Stéphane MD, PhD in Neurosurgery. Published online December 2015 doi:10.1227/NEU.0000000000000993
Abstract
Hypnosis for Awake Surgery of Low-grade Gliomas: Description of the Method and Psychological Assessment
BACKGROUND: Awake craniotomy with intraoperative electric stimulation is a reliable method for extensive removal of low-grade gliomas while preserving the functional integrity of eloquent surrounding brain structures. Although fully awake procedures have been proposed, asleep-awake-asleep remains the standard technique. Anesthetic contraindications are the only limitation of this method, which is therefore not reliable for older patients with high-grade gliomas.
OBJECTIVE: To describe and assess a novel method for awake craniotomy based on hypnosis.
METHODS: We proposed a novel hypnosedation procedure to patients undergoing awake surgery for low-grade gliomas in our institution between May 2011 and April 2015. Surgical data were retrospectively recorded. The subjective experience of hypnosis was assessed by 3 standardized questionnaires: the Cohen Perceived Stress Scale, the Posttraumatic Stress Disorder Checklist Scale, the Peritraumatic Dissociative Experience Questionnaire, and a fourth questionnaire designed specifically for this study.
RESULTS: Twenty-eight questionnaires were retrieved from 43 procedures performed on 37 patients. The Peritraumatic Dissociative Experience Questionnaire revealed a dissociation state in 17 cases. The Perceived Stress Scale was pathological in 8 patients. Two patients in this group stated that they would not accept a second hypnosedation procedure. The Posttraumatic Stress Disorder Checklist Scale revealed 1 case of posttraumatic stress disorder. Burr hole and bone flap procedures were the most frequently reported unpleasant events during opening (15 of 52 events).
CONCLUSION: The main findings of our study are the effectiveness of the technique, which in all cases allowed resection of the tumor up to functional boundaries, and the positive psychological impact of the technique in most of the patients.
“Hypnosis for Awake Surgery of Low-grade Gliomas: Description of the Method and Psychological Assessment” by Zemmoura, Ilyess MD, PhD; Fournier, Eric MD; El-Hage, Wissam MD, PhD; Jolly, Virginie ST; Destrieux, Christophe MD, PhD; and Velut, Stéphane MD, PhD in Neurosurgery. Published online December 2015 doi:10.1227/NEU.0000000000000993







