Therapies that specifically target mutations in a person’s cancer have been much-heralded in recent years, yet cancer cells often find a way around them. To address this, researchers at University of California, San Diego School of Medicine and Moores Cancer Center identified a promising combinatorial approach to treating glioblastomas, the most common form of primary brain cancer.
The study, published May 5 by Oncotarget, demonstrates that a mouse model of glioblastoma and human glioblastoma tissue removed from patients and cultured in the lab can be effectively treated by combining three classes of anti-cancer drugs: a drug that targets a cancer mutation in the Epidermal Growth Factor Receptor (EGFR) gene, a drug that increases stress in cancer cells and a drug that damages cancer cell DNA.
“Developing therapies against glioblastoma is like a chess game. For each therapy administered, or move, by the physician, the cancer makes a counter-move,” said senior author Clark Chen, MD, PhD, associate professor of neurosurgery and vice-chair of Research and Academic Development at UC San Diego.
In up to 50 percent of glioblastomas, mutations in the EGFR gene render cancer cells insensitive to growth regulation by environmental cues, allowing them to grow uncontrollably. Yet highly specific EGFR inhibitors are not particularly effective against glioblastomas with EGFR mutations.
“When glioblastoma cells are treated with EGFR inhibitors, they turn on another receptor to bypass the need for EGFR,” said Chen. “Any hope of an effective treatment requires a combination of moves strategically designed for a checkmate.”
To develop such a strategy, Chen and his group turned to PLK1, a protein that regulates stress levels within glioblastoma cells and is essential for their survival. Chen and his group found that glioblastoma cells that developed resistance to EGFR inhibitors remain universally dependent on this protein.
In mouse models of glioblastoma and in explants of human glioblastoma, singular treatment with an EGFR inhibitor, a PLK1 inhibitor or the current standard of care drug (a DNA-damaging agent), each temporarily halted glioblastoma growth. But, like the human disease, the tumor eventually grew back. However, no detectable tumor recurrence was observed when a combination of all three classes of drugs was administered. The treated mice tolerated this combination regimen without showing significant side-effects.
“It is often assumed that if we find the cancer-causing mutation and inhibit the function of that mutation, we will be able to cure cancer,” said study co-author Bob S. Carter, MD, PhD, chief of neurosurgery at UC San Diego. “Our study demonstrates that the reality is far more complex. Our results provide a blueprint for how to leverage fundamental biologic concepts to tackle this challenging complexity.”
The three drugs administered to mice in this study were: BI2536, a PLK1 inhibitor; Gefitnib, an EGFR inhibitor; and TMZ, the standard-of-care chemotherapy for glioblastoma. The study authors note that while the safety or side effects of treating human patients will all three drugs is unknown, all are individually well-tolerated in humans. The clinical safety profiles of Gefitinib and TMZ are well-established for glioblastoma patients and PLK1 inhibitors have so far been well-tolerated in clinical trials (one has advanced to Phase III clinical trials for acute myeloid leukemia).
Co-authors of this study include Ying Shen, UC San Diego and Shanghai Jiao Tong University; Jie Li, Diahnn Futalan, Tyler Steed, Jeffrey M Treiber, and Zack Taich, UC San Diego; Masayuki Nitta, Dana-Farber Cancer Institute; Deanna Stevens, Jill Wykosky, Frank B. Furnari, Webster K. Cavenee, and Arshad Desai, UC San Diego and Ludwig Cancer Research; Hong-Zhuan Chen, Shanghai Jiao Tong University; Oren J. Becher, Duke University Medical Center; Richard Kennedy, Queen’s University of Belfast; Fumiko Esashi, University of Oxford; and Jann N. Sarkaria, Mayo Clinic.
Funding: This research was funded, in part, by the Sontag Foundation, Burroughs Wellcome Foundation, Kimmel Foundation, Doris Duke Foundation and Forbeck Foundation.
Source: Heather Buschman – UC San Diego Health System
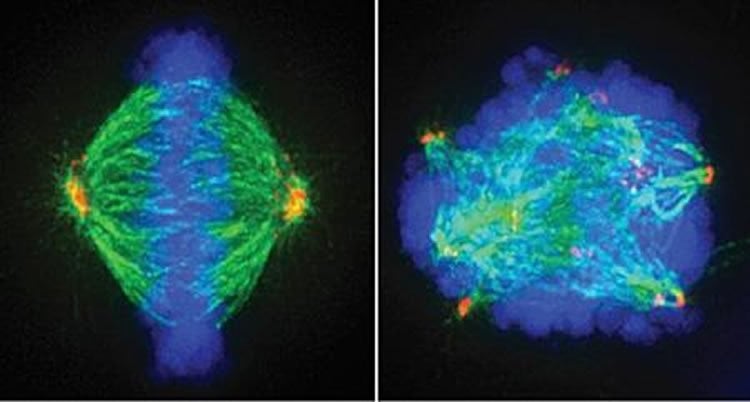
Image Source: The image is credited to UC San Diego Health System
Original Research: Abstract for “Orthogonal targeting of EGFRvIII expressing glioblastomas through simultaneous EGFR and PLK1 inhibition” by Ying Shen, Jie Li, Masayuki Nitta, Diahnn Futalan, Tyler Steed, Jeffrey M. Treiber, Zack Taich, Deanna Stevens, Jill Wykosky, Hong-Zhuan Chen, Bob S. Carter, Oren J. Becher, Richard Kennedy, Fumiko Esashi, Jann N. Sarkaria, Frank B. Furnari, Webster K. Cavenee, Arshad Desai, and Clark C. Chen in Oncotarget. Published online May 5 2015 doi:Unknown
Abstract
Orthogonal targeting of EGFRvIII expressing glioblastomas through simultaneous EGFR and PLK1 inhibition
We identified a synthetic lethality between PLK1 silencing and the expression of an oncogenic Epidermal Growth Factor Receptor, EGFRvIII. PLK1 promoted homologous recombination (HR), mitigating EGFRvIII induced oncogenic stress resulting from DNA damage accumulation. Accordingly, PLK1 inhibition enhanced the cytotoxic effects of the DNA damaging agent, temozolomide (TMZ). This effect was significantly more pronounced in an Ink4a/Arf(-/-) EGFRvIII glioblastoma model relative to an Ink4a/Arf(-/-) PDGF-β model. The tumoricidal and TMZ-sensitizing effects of BI2536 were uniformly observed across Ink4a/Arf(-/-) EGFRvIII glioblastoma clones that acquired independent resistance mechanisms to EGFR inhibitors, suggesting these resistant clones retain oncogenic stress that required PLK1 compensation. Although BI2536 significantly augmented the anti-neoplastic effect of EGFR inhibitors in the Ink4a/Arf(-/-) EGFRvIII model, durable response was not achieved until TMZ was added. Our results suggest that optimal therapeutic effect against glioblastomas requires a “multi-orthogonal” combination tailored to the molecular physiology associated with the target cancer genome.
“Orthogonal targeting of EGFRvIII expressing glioblastomas through simultaneous EGFR and PLK1 inhibition” by Ying Shen, Jie Li, Masayuki Nitta, Diahnn Futalan, Tyler Steed, Jeffrey M. Treiber, Zack Taich, Deanna Stevens, Jill Wykosky, Hong-Zhuan Chen, Bob S. Carter, Oren J. Becher, Richard Kennedy, Fumiko Esashi, Jann N. Sarkaria, Frank B. Furnari, Webster K. Cavenee, Arshad Desai, and Clark C. Chen in Oncotarget. Published online May 5 2015 doi:Unknown doi:10.1523/JNEUROSCI.4489-14.2015






