Possible key to understanding and treating cognitive symptoms of the disease.
A new study has identified a pattern of brain activity that may be a sign of memory problems in people with schizophrenia. The biomarker, which the researchers believe may be the first of its kind, is an important step toward understanding and treating one of the most devastating symptoms of schizophrenia.
The study, led by researchers at Columbia University Medical Center (CUMC) and the New York State Psychiatric Institute (NYSPI), was published today in the journal Biological Psychiatry.
While schizophrenia typically causes hallucinations and delusions, many people with the disorder also have cognitive deficits, including problems with short- and long-term memory.
“Of all the symptoms linked to schizophrenia, memory issues may have the greatest impact on quality of life, as they can make it difficult to hold down a job and maintain social relationships,” said first author Jared X. Van Snellenberg, PhD, assistant professor of clinical psychology (in psychiatry) at CUMC and research scientist in the division of translational imaging at NYSPI. “Unfortunately, we know very little about the cause of these memory problems and have no way to treat them.”
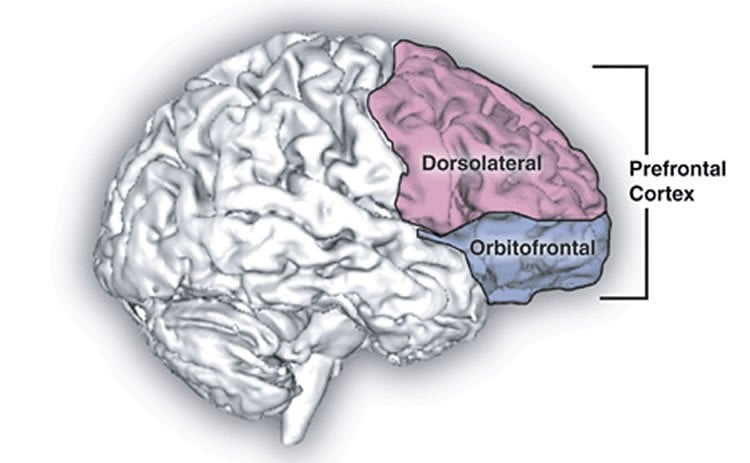
Researchers have long hypothesized that memory problems in schizophrenia stem from disruptions in the brain’s dorsolateral prefrontal cortex (DLPFC). This area of the brain plays a key role in working memory–the system for temporarily storing and managing information required to carry out complex cognitive tasks. However, previous studies, which used functional magnetic resonance imaging (fMRI) to compare DLPFC activation in healthy individuals and those with schizophrenia while taking memory tests, have not shown clear differences.
Dr. Van Snellenberg hypothesized that the studies failed to detect a difference because the memory tests did not have enough levels of difficulty. In 2014 he and his colleagues designed a computerized test that includes eight levels of increasingly difficulty in a single working memory task.
In the current study, 45 healthy controls and 51 schizophrenia patients, including 21 who were not taking antipsychotic medications, were given the eight-level memory test while undergoing fMRI imaging. As expected, the healthy controls demonstrated a gradual increase in DLPFC activation, followed by a gradual decrease in activation as the task gets harder. But in both medicated and unmedicated schizophrenia patients, the overall response was significantly weaker, with the weakest response occurring in those who had the most difficulty with the memory task.
The researchers believe this may be the first time a brain signal in DLPFC has been directly linked to working memory performance in patients with schizophrenia.
“Our findings provide evidence that the DLPFC is compromised in patients with schizophrenia,” said Dr. Van Snellenberg. “What they don’t tell us is why, which is something we ultimately hope to figure out. In the meantime, we now have a specific target for treatment, and a new way to measure whether a treatment is working.”
The study was led by Anissa Abi-Dargham, MD, professor of psychiatry (in radiology) at CUMC and director of the division of translational imaging and of clinical and imaging research in the Lieber Center for Schizophrenia Research at NYSPI.
Funding: The study was supported by grants from the National Institute of Mental Health (1P50MH086404, T32MH018870, 1K01MH107763, and 1K23MH101637) and the National Institutes of Health (5U01MH076544).
Source: Rachel Yarmolinsky – Columbia University Medical Center
Image Source: The image is in the public domain.
Original Research: Abstract for “Mechanisms of Working Memory Impairment in Schizophrenia” by Jared X. Van Snellenberg, Ragy R. Girgis, Guillermo Horga, Elsmarieke van de Giessen, Mark Slifstein, Najate Ojeil, Jodi J. Weinstein, Holly Moore, Jeffrey A. Lieberman, Daphna Shohamy, Edward E. Smith, and Anissa Abi-Dargham in Biological Psychiatry. Published online February 23 2016 doi:10.1016/j.biopsych.2016.02.017
Abstract
Mechanisms of Working Memory Impairment in Schizophrenia
Background
The neural correlates of working memory (WM) impairment in schizophrenia remain a key puzzle in understanding the cognitive deficits and dysfunction of dorsolateral prefrontal cortex observed in this disorder. We sought to determine whether patients with schizophrenia exhibit an alteration in the inverted-U relationship between WM load and activation that we recently observed in healthy individuals and whether this could account for WM deficits in this population.
Methods
Medicated (n = 30) and unmedicated (n = 21) patients with schizophrenia and healthy control subjects (n = 45) performed the self-ordered WM task during functional magnetic resonance imaging. We identified regions exhibiting an altered fit to an inverted-U relationship between WM load and activation that were also predictive of WM performance.
Results
A blunted inverted-U response was observed in left dorsolateral prefrontal cortex in patients and was associated with behavioral deficits in WM capacity. In addition, suppression of medial prefrontal cortex during WM was reduced in patients and was associated with poorer WM capacity in patients. Finally, activation of visual cortex in the cuneus was elevated in patients and associated with improved WM capacity. Together, these findings explained 55% of the interindividual variance in WM capacity when combined with diagnostic and medication status, which alone accounted for only 22% of the variance in WM capacity.
Conclusions
These findings identify a novel biomarker and putative mechanism of WM deficits in patients with schizophrenia, a reduction or flattening of the inverted-U relationship between activation and WM load observed in healthy individuals in left dorsolateral prefrontal cortex.
“Mechanisms of Working Memory Impairment in Schizophrenia” by Jared X. Van Snellenberg, Ragy R. Girgis, Guillermo Horga, Elsmarieke van de Giessen, Mark Slifstein, Najate Ojeil, Jodi J. Weinstein, Holly Moore, Jeffrey A. Lieberman, Daphna Shohamy, Edward E. Smith, and Anissa Abi-Dargham in Biological Psychiatry. Published online February 23 2016 doi:10.1016/j.biopsych.2016.02.017







