The brains of some Iraq and Afghanistan combat veterans who survived blasts from improvised explosive devices (IEDs) and died later of other causes show a distinctive honeycomb pattern of broken and swollen nerve fibers throughout critical brain regions, including those that control executive function. The pattern is different from brain damage caused by car crashes, drug overdoses or collision sports, and may be the never-before-reported signature of blast injuries suffered by soldiers as far back as World War I.
Vassilis Koliatsos, M.D., professor of pathology, neurology, and psychiatry and behavioral sciences at the Johns Hopkins University School of Medicine, recently published a study in Acta Neuropathologica Communications that found survivable blasts may cause hidden brain injuries that play a role in the psychological and social problems some veterans face after coming home.
“This is the first time the tools of modern pathology have been used to look at a 100-year-old problem: the lingering effect of blasts on the brain,” says Koliatsos, senior author of the study that used molecular probes to reveal details in the brains of veterans who died months or years after an IED blast. “We identified a pattern of tiny wounds, or lesions, that we think may be the signature of blast injury. The location and extent of these lesions may help explain why some veterans who survive IED attacks have problems putting their lives back together.”
Soldiers have struggled with bomb-induced brain damage since 1914, when German and Allied forces tried to blast one another out of entrenched positions with monthslong bombardments. Many World War I fighters survived the barrage outwardly unscarred, but with an array of cognitive and psychological difficulties known as shell shock. After World War I, mass bombardments of troops were rare, and shell shock became uncommon. Now renamed blast neurotrauma or blast injury to brain, it has re-emerged due to insurgent forces’ widespread use of IEDs in Iraq and Afghanistan.
To understand this puzzling ailment, a team of eight researchers examined the brains of five male United States military veterans who survived IED attacks but later died. The remains were donated to the Armed Forces Institute of Pathology. Three died of methadone overdoses that could have been accidental, Koliatsos says, since the drug is commonly prescribed to treat soldiers’ chronic pain. One died of a gunshot wound to the head, and one died of multiple organ failure. The researchers compared the veterans’ brains to those of 24 people who died of a range of causes, including motor vehicle crashes, opiate overdoses and heart attacks.
The researchers used a molecular marker to track a protein called APP that normally travels from one nerve cell to another via a long nerve fiber, or axon. When axons are broken by an injury, APP and other proteins accumulate at the breaks, causing swelling. In the brains of people killed in car accidents, the swellings are large and bulb-shaped. In cases of methadone overdose, these axonal swellings are small.
In the brains of four of the five veterans who survived wartime blast injuries, the axonal bulbs were medium-sized and usually arrayed in a honeycomb pattern near blood vessels. “We did not see that pattern in other types of brain injury,” says Koliatsos.
The veterans’ brains did not show signs of the neurodegenerative disease known as punch-drunk syndrome, which is caused by multiple concussions. But near the damaged axons, a second molecular probe revealed specialized cells, called microglia, that are involved in brain inflammation.
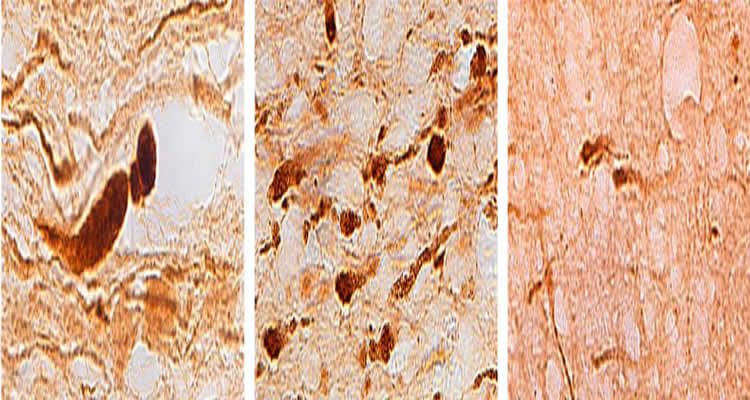
“In brains that had been exposed to blasts, we see microglial cells right next to these unusual axonal abnormalities,” Koliatsos says. Brain inflammation develops slowly, so microglia don’t normally appear in drug overdose cases. Their presence suggests the veterans who overdosed had pre-existing brain injuries.
The researchers found these distinctive lesions in a number of places in veterans’ brains, including in the frontal lobes, which control decision making, memory, reasoning and other executive functions. The lesions may be fragments of nerve fibers that broke at the time of the blast and slowly deteriorated, or they may have been weakened by the blast and broken by some later insult like a concussion or drug overdose.
“When you look at a brain, you are looking at the life history of an individual, who may have a history of blasts, fighting, substance abuse or all of those,” Koliatsos says. “If researchers could study survivors’ brains at different times after a blast — a week, a month, six months, one year, three years —that would be a significant step forward in figuring out what actually happens over time after a blast.”
A century after the first reported cases of shell shock, the struggle to overcome this invisible injury continues. Doctors treating IED survivors “often see depression, anxiety, post-traumatic stress, and substance abuse or adjustment disorders. Life is very difficult for some of these veterans,” says Koliatsos. “It’s important to understand that at least a portion of these difficulties may have a neurological foundation.”
This research was funded by the Johns Hopkins Alzheimer’s Disease Research Center (Grant RFA AG-09-001) and gifts from the Kate Sidran Family Foundation and the Sam and Sheila Geller family.
Other authors on the paper are Jiwon Ryu, Leyan Xu, Olga Pletnikova, Francesco Leri, Charles Eberhart and Juan C. Troncoso of the Johns Hopkins University School of Medicine and Iren Horkayne-Szakaly of the Veterans Administration Medical Center in Washington, D.C.
Contact: Heather Dewar – Johns Hopkins Medicine
Source: Johns Hopkins Medicine press release
Image Source: The image is credited to Vassilis Koliatsos and is adapted from the Johns Hopkins Medicine press release
Original Research: Full open access research for “The problem of axonal injury in the brains of veterans with histories of blast exposure” by Jiwon Ryu, Iren Horkayne-Szakaly, Leyan Xu, Olga Pletnikova, Francesco Leri, Charles Eberhart, Juan C Troncoso, and Vassilis E Koliatsos in Acta Neuropathologica Communications. Published online November 25 2014 doi:10.1186/s40478-014-0153-3






