Summary: The amount of amyloid plaques present within a person’s brain can indicate the rate at which their cognition will decline in the following four years, a new study reports.
Source: UT Dallas.
Increased amyloid plaque leads to increased cognitive decline, according to Center for Vital Longevity Scientists.
A new study from the Center for Vital Longevity at The University of Texas at Dallas has found that the amount of amyloid plaques in a person’s brain predicts the rate at which his or her cognition will decline in the next four years.
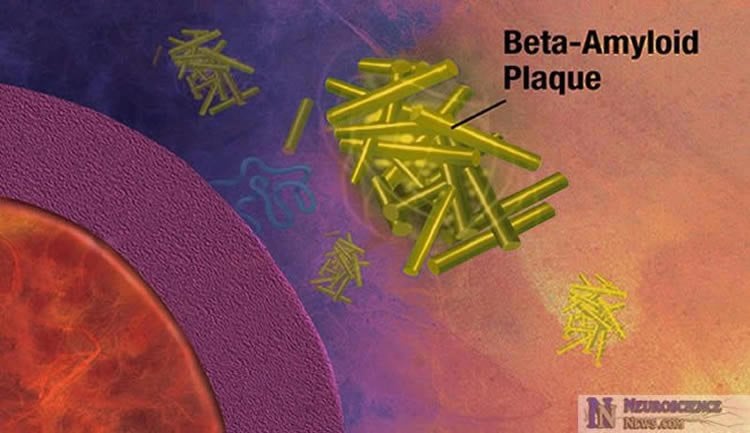
The study, published in JAMA Neurology, used positron emission tomography (PET) scans to detect amyloid in 184 healthy middle-age and older adults participating in the Dallas Lifespan Brain Study. Amyloid plaques, a sticky buildup that gradually gathers outside of neurons and is a hallmark of Alzheimer’s disease, are believed to start accumulating in the brain 10 to 20 years before the onset of dementia.
“We think it is critical to examine middle-aged adults to detect the earliest possible signs of Alzheimer’s disease, because it is becoming increasingly clear that early intervention will be the key to eventually preventing Alzheimer’s disease,” said Michelle Farrell, a PhD student at the center and the lead author of the study.”
The study presents some of the first data on amyloid and its cognitive consequences in adults ages 40 to 59. For these middle-age adults, the study found that higher amyloid amounts were associated with declines in vocabulary, an area of cognition that is generally preserved as people age.
The results suggest that a new approach might be needed to provide physicians and patients with information about the future for someone with amyloid deposits. Amyloid PET scan results are typically presented as either positive or negative, but the new findings suggest that the amount of amyloid in the brain provides useful prognostic information about how rapidly cognition may decline in the future.
“Our understanding of the earliest and silent phase of possible Alzheimer’s disease is increasing rapidly. Providing physicians and patients with more information about the magnitude of amyloid deposits will provide valuable information that will permit better planning for the future,” said Dr. Denise Park, director of research at the Center for Vital Longevity, Distinguished University Chair in Behavioral and Brain Sciences and senior author of the study.
Park heads up the Dallas Lifespan Brain Study, which is a multi-year research project aimed at understanding what a healthy brain looks like and how it functions at every decade of life from age 20 through 90. Each of the nearly 500 volunteers in the study undergo tests every four years.
While most studies of amyloid and its relationship to Alzheimer’s disease have focused on older adults over age 60, the Dallas Lifespan Brain Study also studies middle-age adults to find the earliest possible signs of Alzheimer’s disease.
In the JAMA Neurology research, the three middle-age adults who had the highest amyloid amounts and greatest vocabulary decline were also found to have a double dose of the ApoE-4 gene implicated in Alzheimer’s. This means they received a copy of the gene from each of their parents. Only about 4 percent of the population carries this genetic combination, and the finding hints at the possibility that subtle symptoms of cognitive decline related to amyloid may be detectable as early as middle age in this vulnerable population.
Funding: The study was funded by the National Institute on Aging, and additional support was provided by Avid Radiopharmaceuticals, a subsidiary of Eli Lilly, which developed florbetapir, a radiotracer that, along with PET imaging, measured amyloid deposits.
Source: Alex Lyda – UT Dallas
Image Source: NeuroscienceNews.com image is in the public domain.
Original Research: Full open access research for “Association of Longitudinal Cognitive Decline With Amyloid Burden in Middle-aged and Older Adults: Evidence for a Dose-Response Relationship” by Michelle E. Farrell, BA; Kristen M. Kennedy, PhD; Karen M. Rodrigue, PhD; Gagan Wig, PhD; Gérard N. Bischof, PhD; Jennifer R. Rieck, PhD; Xi Chen, MS; Sara B. Festini, PhD; Michael D. Devous Sr, PhD; and Denise C. Park, PhD in JAMA Neurology. Published online May 30 2017 doi:10.1001/jamaneurol.2017.0892
[cbtabs][cbtab title=”MLA”]UT Dallas “More Amyloid in the Brain, More Cognitive Decline.” NeuroscienceNews. NeuroscienceNews, 15 June 2017.
<https://neurosciencenews.com/amyloid-cognitive-decline-6922/>.[/cbtab][cbtab title=”APA”]UT Dallas (2017, June 15). More Amyloid in the Brain, More Cognitive Decline. NeuroscienceNew. Retrieved June 15, 2017 from https://neurosciencenews.com/amyloid-cognitive-decline-6922/[/cbtab][cbtab title=”Chicago”]UT Dallas “More Amyloid in the Brain, More Cognitive Decline.” https://neurosciencenews.com/amyloid-cognitive-decline-6922/ (accessed June 15, 2017).[/cbtab][/cbtabs]
Abstract
Association of Longitudinal Cognitive Decline With Amyloid Burden in Middle-aged and Older Adults: Evidence for a Dose-Response Relationship
Importance Presently, the clinical standard for reporting the results of an amyloid positron emission tomography scan is to assign a dichotomous rating of positive or negative for the presence of amyloid. In a 4-year longitudinal study, we investigated whether using a continuous measure of the magnitude of baseline amyloid burden would provide valuable information about the rate of future cognitive decline over the subsequent 4 years compared with a dichotomous measure in middle-aged and older adults.
Objective To examine whether a continuous, dose-response relationship between amyloid burden and cognitive decline was present among middle-aged and older adults.
Design, Setting, and Participants This cohort study included 174 participants from the Dallas Lifespan Brain Study who were 40 to 89 years old at the beginning of the study, were cognitively normal at baseline (a Mini-Mental State Examination score of 26 or higher) with no history of neurological or psychiatric disorders, and had completed amyloid imaging ([18F]-florbetapir) at baseline and cognitive assessments at baseline and a 4-year follow-up. Continuous amyloid burden was measured as the mean cortical standardized uptake value ratio (SUVR) at baseline.
Main Outcomes and Measures Linear mixed models assessed the effect of increasing baseline amyloid over time (SUVR × time interaction) on episodic memory, reasoning, processing speed, vocabulary, and Mini-Mental State Examination performance. Age, sex, education, apolipoprotein ε4, and the random effect of intercepts were included as covariates.
Results The mean (SD) age for all participants (n = 174) was 66.44 (11.74) years, and 65 participants (37%) were men. The primary analyses yielded significant SUVR × time interactions in episodic memory, processing speed, vocabulary, and Mini-Mental State Examination performance, but not in reasoning performance. Higher baseline SUVR projected greater cognitive decline over 4 years. When controlling for variance related to a dichotomized positive/negative classification, most effects on cognition remained. Dichotomized amyloid status alone yielded fewer significant effects of amyloid on cognitive decline than continuous SUVR. Among amyloid-positive participants, increasing baseline SUVR predicted an increasing decline in episodic memory, but other effects on cognition were more limited. Finally, higher baseline amyloid burden among middle-aged adults was related to changes in vocabulary, with the effect driven by 3 apolipoprotein ε4 homozygotes.
Conclusions and Relevance These results suggest that the magnitude of amyloid burden at baseline is associated with the rate of cognitive decline over 4 years and potentially provides important information about the rate of future cognitive decline that is not available from a dichotomous positive/negative categorization.
“Association of Longitudinal Cognitive Decline With Amyloid Burden in Middle-aged and Older Adults: Evidence for a Dose-Response Relationship” by Michelle E. Farrell, BA; Kristen M. Kennedy, PhD; Karen M. Rodrigue, PhD; Gagan Wig, PhD; Gérard N. Bischof, PhD; Jennifer R. Rieck, PhD; Xi Chen, MS; Sara B. Festini, PhD; Michael D. Devous Sr, PhD; and Denise C. Park, PhD in JAMA Neurology. Published online May 30 2017 doi:10.1001/jamaneurol.2017.0892






